How to set an achievable goal for 2024
“Life is short, fragile and does not wait for anyone. There will never be a perfect time to pursue your dreams and goals. ” – Unknown.
Did you start 2024 with a goal? Eating more healthfully, quitting smoking, exercising regularly, learning a new skill, changing careers, buying a house?
If so, you’re not alone. Lots of us start a new year with lofty goals, wanting to start fresh. It’s like the first day of school when you’d open a brand new notebook, and it felt so bright and shiny with endless possibilities (aaah, new stationery 😉).
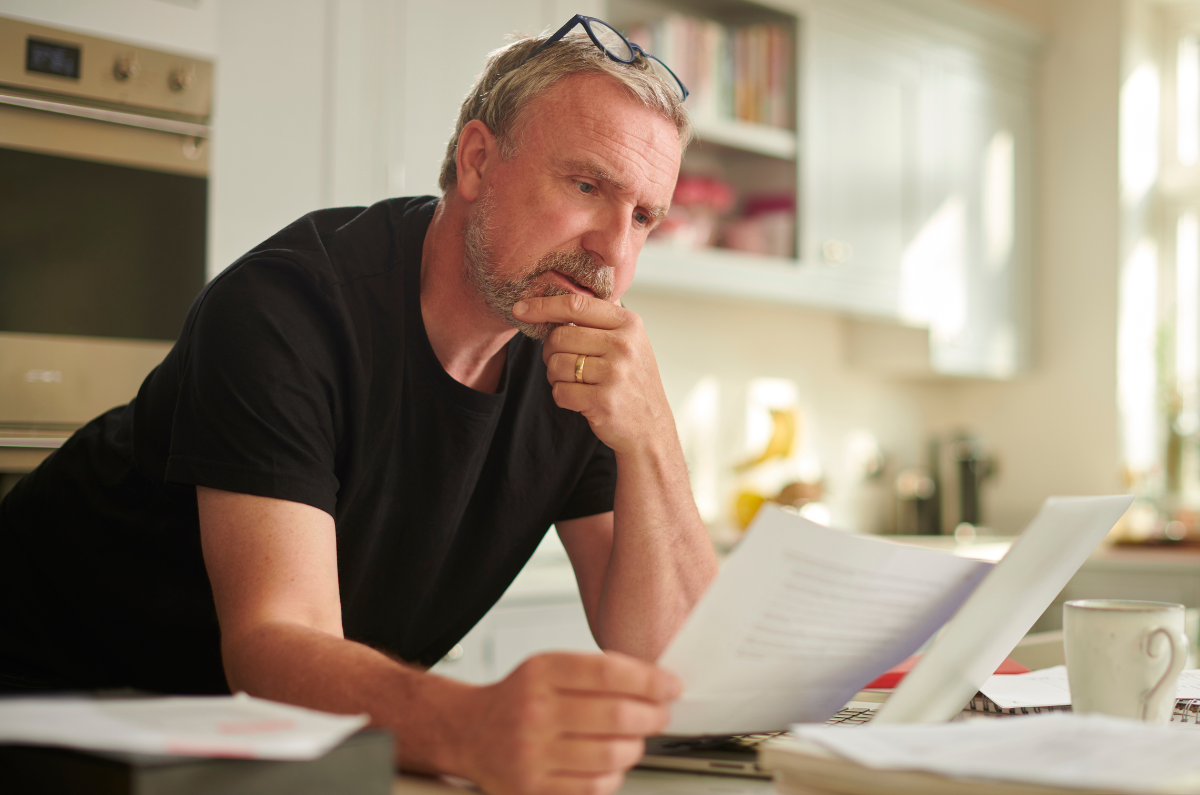
And we start on our path with gusto – we try new recipes, visit the Quit website, pull the walking shoes out of the cupboard. But then life interferes. A tough day at work leads to takeaway for dinner instead of cooking. You’re out with mates, and everyone’s smoking, so you do too. You wake up exhausted and toss your walking shoes back into the cupboard. The enthusiasm for achieving your goal wanes.
So why bother with goals? What’s the point if they can be hard to achieve?
Simply put, having goals gives us control in a world where so much is out of our control. They provide us with something to work towards, and give us the steps we need to get there.
So let’s look at some simple ways you can live your life and still achieve your goals.
First – let’s address the elephant in the room. It starts with ‘C’ and ends in ‘OVID’.
We’re living in a global pandemic, and we’re a little tired. Two years of pandemic fatigue, fear, stress, and worry mean our physical and mental energy levels are lower than they’ve ever been.
These feelings can’t be ignored or pushed aside in order to achieve your goals. They need to be acknowledged and factored into your goal setting.
Make your goals meaningful
When setting a goal, think of something important to you and not something you think you should do. You’re more likely to be successful if you aim to do something that makes you happy and has meaning. And you’ll be more likely to recover from stumbles or overcome obstacles if your goal is significant to you.
Start with small goals
When we set ourselves a goal we often begin with great excitement, but then something – pain, work, illness, family life, pandemic-life – gets in the way. However if we create small goals, we’re putting ourselves in a better position to succeed.
For example, say you want to read more books. Great! There are so many amazing books out there. But having the goal of reading a book a week may not be realistic (been there done that 😆).
A more feasible way to read more books is to read a chapter in the evening. Or read for 15 minutes in the morning. You’re still reading, but it’s a smaller, more realistic goal.
Be flexible
If you’re having difficulties achieving your goal, ask yourself why? If it has meaning for you and it’s realistic, what’s the barrier? If we use the reading example again, it could be that you can’t find the time to sit and read. Or your eyes are tired after staring at a computer screen all day.
A way to solve this problem could be to listen to audio books. You can do this while doing other things, and your tired eyes don’t have to focus on the words. You can access many titles free through your public library, or you can access a subscription service such as Audible.
The point is that if you’re flexible, there are ways you can still achieve your goal if the original plan didn’t work. Discuss it with family or friends if you can’t think of solutions. Talking through the issue can help you gain some clarity. And the support and advice from the people who care for us is invaluable.
Be kind
When working towards a goal, it’s realistic to expect that there’ll be some trips and stumbles along the way. When this happens, be kind to yourself. When things don’t go according to our plans, we can be very critical. So avoid berating yourself. Instead, look at the stumble as a chance to learn. What happened? Why did it happen? How can you avoid it happening again? Does your goal need some adjustment to make it more achievable?
Another thing to remember is that we’re all different. So don’t compare yourself with others. This can be tough when you’re surrounded by carefully curated, touched up and filtered images, stories and posts about people who seem to have it all together, while you feel like a red hot mess (hmm, that may be just me?). But comparing yourself to others won’t help you achieve your goal and can make you feel like you’re failing somehow. So avoid these comparisons, be kind to yourself and give yourself credit for doing your best.
Be SMART
A common acronym used for goal setting is SMART: Specific, Measurable, Achievable, Realistic and Timeframe. It can help you create a goal that works for you and your life.
Be specific. What is it you’re aiming for? Ask yourself the 5 W’s – who, what, when, where, why. What do you want to accomplish? Why? When and where will you do this? Who can help you?
Let’s use meditation as an example to create a SMART goal. You enjoy meditating. It helps you manage your pain and deal with anxiety. So in 12 months, you’d like to be meditating for 30 minutes a day, 5 days a week.
You need to be able to measure your goal so that you know when/if you’ve achieved it. Meditating more often isn’t a measurable goal, but committing to meditating for a specific amount of time in a day is.
Next, your goal needs to be achievable for you. It should challenge you and stretch you a little but still be attainable, especially considering the uncertainties of the world we’re living in.
Planning to meditate for 60 minutes every day probably isn’t achievable, especially if you’re just starting out. But committing to meditate 10 minutes a day, twice a week is. You can increase the amount of time and the number of days you meditate as you progress.
You need to be realistic, and your goal needs to be doable – for you and your own circumstances. Meditating 10 minutes a day, twice a week is realistic because you enjoy it, and it helps you relax. You’ve discussed it with your family, and they understand that they can’t interrupt you during this time. You’ve organised a quiet space to meditate, and you’ve downloaded a meditation app that you like. You’re committed, and you’ve put in place the things you need to make your goal possible. That makes your goal realistic.
Finally, your goal should have a timeframe. In this example, your goal is to meditate for 30 minutes, 5 days a week in 12 months. You’ll be starting at 10 minutes a day, twice a week increasing this over the coming 12 months. A timeframe gives you motivation and an endpoint to work towards.
Sticking to it
Once you’ve decided on your goal, write it down, along with the steps you need to get there. Stick it on your fridge, bathroom mirror or somewhere you’ll see it often. Refer to it regularly. And remember, if you have any hiccups along the way, that’s okay. Just don’t give up. Learn from what happened and move on.
“I hope that in this year to come, you make mistakes. Because if you are making mistakes, then you are making new things, trying new things, learning, living, pushing yourself, changing yourself, changing your world. You’re doing things you’ve never done before, and more importantly, you’re doing something.” —Neil Gaiman.
Originally written and published by Lisa Bywaters 19 January 2022.
Contact our free national Help Line
If you have questions about managing your pain, your musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services be sure to call our nurses. They’re available Monday to Thursday between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore